Attracting and retaining staff, reducing bed block, sharing resources and increased access to specialists are among the benefits of a co-located hospital in Launceston - according to the surgeons who have been advocating the idea for decades.
Subscribe now for unlimited access.
or signup to continue reading
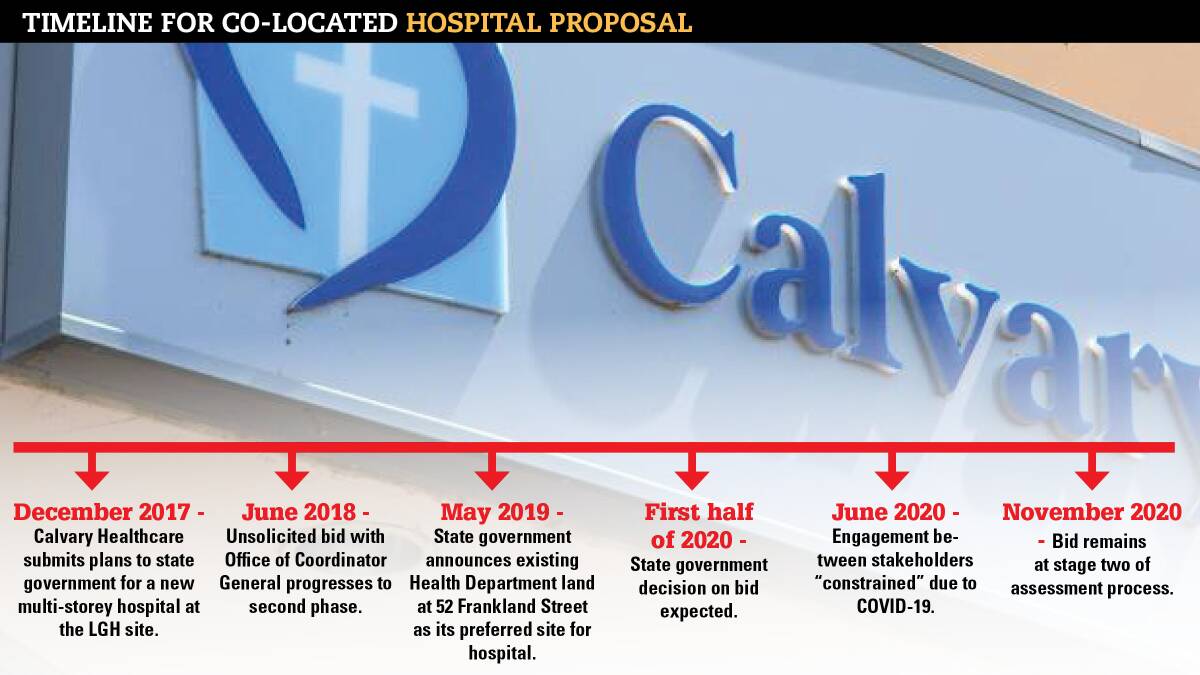
More than three years after it was put to the state government, Calvary Healthcare's unsolicited bid for a co-located hospital remains at stage two with the Office of the Coordinator-General.
But for orthopaedic surgeon Dr John Batten and urological surgeon Dr Mike Monsour, the concept has been on the cards for the better part of two decades.
The pair were among a small group of specialists who initially canvassed the idea of a co-located health precinct at the Launceston General Hospital about 22 years ago.
Now, with a $100 million commitment from Calvary to get the proposal off the ground, they have weighed in on how the development could fundamentally change the way healthcare is delivered in Northern Tasmania and help tackle the needs of an ageing population and rising rates of chronic disease.

What is a co-located hospital?
A co-located model enables healthcare providers to share the same campus or building, along with the specialists, services and resources they provide.
The state's south already has a co-located arrangement, with the Royal Hobart Hospital operating in a co-located relationship with the Hobart Private Hospital.
Similarly, the North-West Private Hospital is located alongside the North West Regional in Burnie.
Yet as it stands, Launceston has very limited private hospital services compared to similar regional cities in other states.
Up to a third of patients who present to the LGH are also estimated to have private health insurance.
However, they often present to the public hospital because of a lack of private services elsewhere.
Dr Monsour - the former chairman of Calvary's medical advisory committee - said co-located hospital arrangements were becoming increasingly more common around the world.
However, he said adequate staffing and integration remained one of the keys to their success.
"There's always been concerns in the past, with co-located concepts, that it's going to fail because it becomes two separate hospitals on one site, but they are still functioning independently, rather than in a cooperative manner," he said.
"But where it's worked, it's because they've identified that there are needs - especially in a regional area - that shouldn't be duplicated.
"We also know for co-location to work, you have to ensure adequate staffing - especially nursing staff. Tasmania has ageing nurses in both the public and private systems.
"So, we need to encourage and retain the new young nurses from looking for work interstate. A co-located arrangement would go a long way in securing this."

When it comes to Calvary's bid, a new co-located hospital would replace the private healthcare provider's existing two hospital sites - St Luke's, on Lyttleton Street, and St Vincent's, on Frederick Street.
The state government has already earmarked existing health department land at 52 Frankland Street - across from the LGH - as its preferred site for a co-located hospital.
It's a location Dr Monsour also supports, with the position favouring access to the LGH emergency department, operating theatres, intensive care unit, radiology and pathology services.
Considering existing limitations facing private patients in Launceston - including the more than 11,700 public patients awaiting elective surgery across Tasmania - he said the benefits of co-located services would be substantial for both the community and medical professionals alike.
"Complicated surgical or interventional medical procedures that require post-operative ICU care cannot be accommodated at Calvary campuses and requires LGH admission and theatre utilisation," he said.
"It is estimated that approximately 25 per cent of patients through the LGH are privately insured and their utilisation of a ward bed and theatre session disadvantages the public patient waiting for access to a bed and surgery.
"The ability to treat these high-risk private patients in a co-located private facility with proximity access to LGH ICU and specialised care is of added benefit to those on the public waiting list."

Attracting and retaining staff
On a national scale, the majority of services provided by many specialists occur outside of the public hospital setting.
Northern Tasmania also has a long and well-recorded history of struggling to attract and retain health professionals.
A recent online survey with more than 1300 StLukesHealth members found 89 per cent would like to see other services accommodated at a new co-located private hospital.
A further 92 per cent said it was important for a new private hospital and the LGH to co-operate and share resources, while 90 per cent agreed a new co-located hospital would enable the region to attract and retain more specialists.
Dr Batten, who retired in 2019 after working as a visiting medical officer in orthopaedics at the LGH for more than 30 years, said the majority of the hospital's workforce consisted of just that - visiting medical officers who share their time between the public and private systems.
He said the consequence was a workforce who often had to juggle their priorities - responding to increased demand while travelling between facilities.
"We are serving a very similar population and often have to be in two places at once," he said.
"It's very important that the services are exceptional for a regional town of our size and I think they can be expanded with closer associations between the public and private.
"Co-location offers advantages for the medical workforce, the nursing workforce, paramedical - physio, occupational therapy - they are all travelling across town to service the private system as well.
"From the patients' point of view, which is probably more important, they will have the ability to get the attention immediately of specialists who are normally out in private, who may be either on call or are available to help negotiate what is required in the management of the patient who presents at the LGH.
"To have them in the same precinct, that is enormously helpful."
Better outcomes for patients
Calvary has been a part of the Tasmanian health system for more than 80 years and says it's committed to evolving to meet contemporary health needs, while fostering positive working relationships between the private and public sectors.
While internal stakeholder consultation of the proposal has reportedly occurred, the scope of services that could be potentially offered through a co-located agreement remains largely unknown.
However, previous reports have indicated a state-of-the-art operating suite, a palliative care unit and rehabilitation unit, an extended hours health clinic and an endoscopy suite could be among some of its features.
Dr Batten said a co-located arrangement made good sense economically, with benefits for both public patients and those with private health insurance.
"The sharing of resources in a small regional town like Launceston is vital," he said.
"There are a group of people, for many reasons, who are not done in private because we do not have advanced care.
"In that case, if they had private insurance, they would be able to access services in a co-located set up, because we would share those very special facilities.
"Further, institutions like intensive care, operating theatres - all of those things are incredibly expensive to run.
"Within a co-located campus, it means more people who might not have been considered appropriate for a private hospital, the service could be done knowing those advanced facilities are close by, rather than across town or requiring an ambulance ride."
Similarly, Dr Monsour said a co-located campus could help address longstanding issues of bed block at the LGH.
A 2019 snapshot survey from the Australasian College of Emergency Medicine found the LGH was the country's worst-performing hospital for patient access block.
Access block occurs when admitted patients needing a hospital bed are delayed from leaving the emergency department because of a lack of inpatient bed capacity.
Dr Monsour said one of the answers was to free up more beds by getting private patients out of the public hospital setting.
"It's a sign of the times when we do grand rounds now and we go and see a cohort of our post-op patients, who are still in casualty," he said.
"They've come into casualty, had their operation and they're still there post-cooperatively in a cubicle with no ward or bed for them. That's wrong.
"I never thought I would practice and see the day when patients in casualty are being fed their breakfast and dinner because there's no bed in the wards.
"But if we can get private patients out of the public system and into the private hospital, we can have more beds, we can get patients out of casualty and we can get a better throughput for the public patients as well."
What could a co-located model bring for the community?
Andrea Selleck, chief executive of the Australian Regional Health Group, has worked in the private health sector for more than 25 years.
Formed in 1995 by a group of health insurance funds operating in predominantly regional areas, ARHG's primary role is to negotiate hospital purchase provider agreements on behalf of its members' funds - including StLukesHealth.
In considering the views expressed by StLukes' members in the recent survey, Ms Selleck said the expectations of Northern Tasmanians with private health insurance were the same as most privately insured Australians.
They include: convenient access to safe and quality care; choice around when and where to have elective surgery and who does it; access to appropriate care at the beginning and end of life; support after discharge; and assistance with managing their health.
She also believes the benefits of a private co-located hospital in Launceston would be significant, including the possibility of further investments back into the health system.
"Calvary is running two separate sites in Launceston so efficiencies can already occur simply by merging the two facilities into one," she said.
"Add to this a truly co-operative arrangement with the public hospital and there will be even greater efficiencies through the shared services model.
"Savings could be considerable, and that money could then be reinvested back into the hospitals to create better services for the members and better opportunities for health professionals.
"This aligns with Calvary's ethos, plus they have considerable experience in running both public and private hospitals."
Ms Selleck also pointed to the success of Hobart's co-located arrangement, including the opportunity that comes with new infrastructure.
"Over the years, many private and public hospitals have had to make do with add-ons and extensions that create more beds, but don't always create operational efficiencies or an improved patient experience," she said.
"A well-designed public/private hospital will be ergonomic and practical to work in, more efficient in terms of operational costs, and will provide a much better experience for the patient, particularly if it hosts the latest in medical technology.
"All of these objectives are much easier to achieve, and much less costly when starting from scratch.
"This will attract doctors, educators and other health professionals - not only Tasmanians who want to practice in their own state, but also professionals from the mainland, particularly given how closely located the two areas are."
- This article is part of a six-week series Critical Condition exploring the what the future of health service delivery in Northern Tasmania looks like.